A ReLACSing Blog #5: Random Reflections from the 2022 Annual Meeting of the American Academy of Neurology
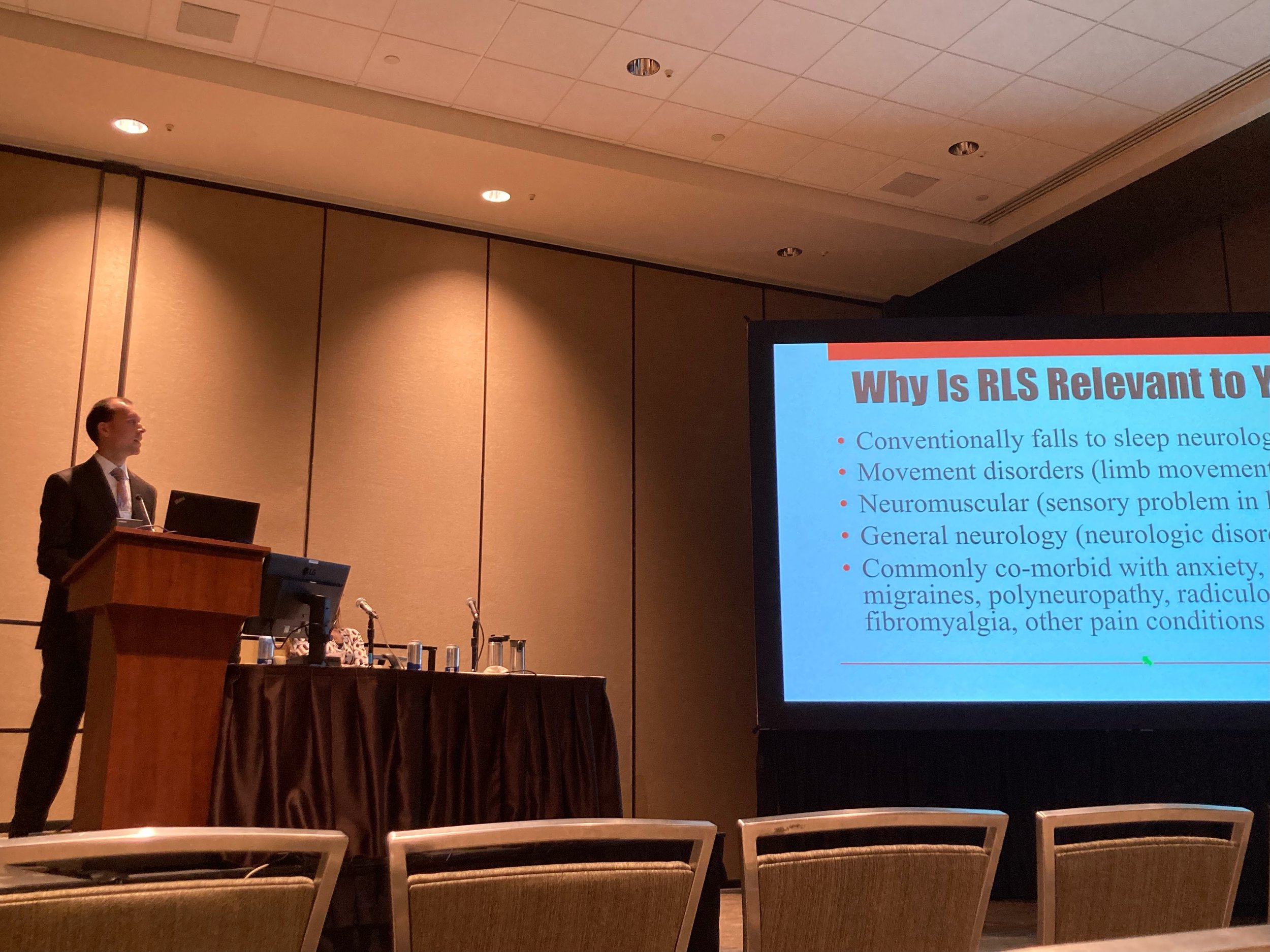
This week, I had the pleasure to attend and present at the American Academy of Neurology’s (AAN) 2022 Annual Meeting in Seattle, WA, the first in-person conference I have attended since before the pandemic. I presented “The Compulsive Use of Dopamine Agonists for Restless Legs Syndrome: 21st-century RLS Management” at C-94 Clinical Approach to Sleep Disorders. This talk had been scheduled for spring of 2020 in Toronto, but that attempt coincided with the COVID-19 lockdown, so no road trip through Canada. These are my scattered observations from the week at the conference:
Dr. Berkowski’s talk was too animated even for the bravest of neurologists to sit court-side in the first row while imploring them to stop prescribing dopamine agonists for RLS.
As neurology becomes more specialized over time, it seems like the conference moved toward more basic knowledge within the subspecialties, with the audience being geared toward students, residents, and fellows, as well as those neurologists within other subspecialties who wanted to crossover and learn about another subspecialty. Thus, some of the sleep medicine was more basic than expected, but there were still a lot of fantastic presentations here.
A whopping three of my other fellowship colleagues and one of my former attending physicians made presentations:
Yasemin Tashman, MD presented on updates to sleep apnea (OSA) including an interesting small study showing that a combination of atomoxetine (Strattera) and oxybutynin (Ditropan) significantly improved sleep apnea when taken together two hours before sleep. The former drug is a mild stimulant used for ADHD but sometimes in sleep medicine for wakefulness and to reduce cataplexy from narcolepsy type 1. Oxybutynin is a drug frequently used to relax bladder muscles to prevent the urge to urinate. Apparently the combination of these two led to improved upper airway muscle function and increased drive to breathe, so this is another non-mechanical attempt to help with a largely mechanical disorder. The mechanical treatments like the first line positive airway pressure (PAP) therapy and the second-line mandibular advancement devices/oral appliance therapies (MAD/OAT) are not always well-tolerated. Weight loss as a treatment takes a long time and also may not always resolve the condition so alternative treatments for OSA are in high demand. I wonder about the effects however, of taking a mild stimulant before bed, though oxybutynin is frequently taken before bedtime for nighttime urination, which is often due to OSA in the first place!
Michelle Jonelis, MD presented a practical approach to behavioral interventions for neurologists to improve insomnia. Preaching to the choir with me, she highlighted that “sedation is not sleep”, a phrase made famous by Matthew Walker, PhD in Why We Sleep and the lack of effectiveness of sleeping pills over cognitive and behavioral interventions. I will be applying these same strategies to treatment of insomnia within ReLACS Health as well. Because sleep is such a natural process, of which evolution has preserved about 7-8 hours per day, there really are no biological disorders that cause insomnia and most disruption of sleep can be reversed by steady, dedicated work on the cognitive and behavioral aspects of sleep, something that the direct specialty care approach will enable, in terms of time and flexibility of scheduling.
Logan Schneider, MD addressed sleepiness and fatigue in “How to Think about Your Sleepy Patient” again focusing on lifestyle and behavioral modifications to sleep. I particularly enjoyed the refresher on RISEUP, from Kate Kaplan, Phd in her 2018 study with: Refrain from snoozing, Increase activity in the first hour, Shower or wash with cold water, Expose yourself to sunlight, Upbeat music, and Phone a friend. Many of us were following this during the conference, particularly with getting up early and seeing so many friends, with the exception of the upbeat music in the conference center, I guess.
Emmanuel Mignot, MD, PhD presented initial findings on TAK-925 a hypocretin stimulating drug delivered through an IV infusion that enabled patients with idiopathic hypersomnolence (IH) to maintain wakefulness for impressive extended periods of time on the maintenance of wakefulness testing. It will be interesting to see if this drug can be made in an oral or other form that can be taken at home and whether it will be as effective. IH, however, is a diagnostic classification, as the name would suggest, that has an unclear biological underpinning. Unfortunately, as I will describe in detail in future blogs, most of the time it is a misdiagnosis of patients who actually are sleepy or sleeping excessively due to disruption of their biological clock, poor sleep quality, the use of medications that cause drowsiness, etc. rather than an “idiopathic” cause. Nevertheless, it does present optimism for other conditions in which sleepiness may not be correctable such as narcolepsy type 1 and shift-work disorder among others.
Perhaps the most important part of national conferences, more than the presentations and scientific knowledge themselves, is the social networking by reconnecting with old colleagues and meeting new people in the field. It was great to be back in person, as virtual conferences were nearly devoid of the personal interaction, though maybe sufficient for the dissemination of information. Unfortunately, the lawyers must have gotten to the AAN planning committee as they enforced draconian “safety” protocols for this conference. Despite plummeting infection rates, they insisted until the end on not only mandatory vaccinations but a booster dose to attend the conference. Thus, you can see ICU or ER patients, perform surgery, etc. at many hospital systems throughout the country without a booster vaccine, but AAN felt that a group of healthy, vaccinated neurologists at a professional conference should be even “safer” and should not enter without a booster dose. Of course, natural immunity was not mentioned in their algorithm, though there are no drug companies to profit from natural immunity. To double down on the scientific meeting not “following the science”, they then topped off the booster mandate with mask mandates! Well, except if you’re eating, drinking, or speaking at the conference, because viruses stand pat during those activities, but they can spread when you’re sitting and watching. Of course, most everyone walked to their conference hotels a block away and could be around the exact same people without masks in the hotel lobby. Among the many drawbacks to masking unnecessarily, I discovered it is very hard to identify people you have only met a few times if they’re all wearing masks. It is quite socially disruptive, and I spent considerable time in RoboCop mode, analyzing the eyes, ears and hair of individuals and then scanning the name tags to see if it was someone I knew or wanted to say hi to. Fortunately, the Associated Professional Sleep Societies’ 2022 Annual Meeting reports they are just going to follow the local health policies at the time of the conference in Charlotte, this June, rather than making the requirement a 5th booster dose + daily PCR testing + PAPR to get into the doors of its conference.
Lastly, the downtown Seattle area, even without going to Pike’s Place, was bustling with walkable streets, restaurants, and shops, but the 40s and drizzle at times made me feel right at home in Michigan. Charlotte in June will hopefully be warmer!!
-Andy Berkowski, MD, neurologist
ReLACS Health